Claire Snape (audioloog bij het Royal Derby Hospital) heeft geen rechtlijnige carrière in de audiologie achter de rug. Na haar schoolopleiding en eindexamen wilde ze gaan studeren, maar ze werd niet toegelaten tot de opleiding van haar eerste keuze. Ze was vastbesloten om in de gezondheidszorg te gaan werken en nam een baan in een ziekenhuis aan terwijl ze haar opties onderzocht. Aanvankelijk overwoog ze logopedie of fysiotherapie.

Toevallig stelde een collega audiologie voor, en in die tijd, in 1997, kon je nog steeds via een stage in het beroep instappen in plaats van via een universitaire opleiding. Claire greep deze kans met beide handen aan en volgde een opleiding aan de School of Audiology in Nottingham, waar ze praktijkervaring opdeed in combinatie met een studie medische fysica aan het People's College. Dankzij de stage kon ze vanaf dag één direct praktijkervaring opdoen en hoefde ze geen collegegeld te betalen.
Ze bouwde haar carrière verder uit in Nottingham, voordat ze in 2004 naar Derby verhuisde, waar haar focus zich uitbreidde van hoortoestellen naar vestibulaire diagnostiek en revalidatie. Tegenwoordig werkt Claire als onderdeel van een toegewijd multidisciplinair team, dat uitgebreide evenwichts- en gehoorzorg biedt en helpt bij het ontwikkelen van gestroomlijnde klinieken waar audiologen en KNO-specialisten samenwerken aan patiëntgerichte oplossingen.
De patiënten en uitdagingen van vestibulaire zorg
Claire legt uit dat het soort patiënten dat ze ziet in de loop der tijd is veranderd. Vroeger kwamen gevallen van labyrinthitis en vestibulaire neuronitis vaker voor, maar de laatste tijd merkt ze een toename van het aantal patiënten met Persisterende Positionele Perceptie Duizeligheid (PPPD)Deze patiënten zijn vaak complexer, omdat ze mogelijk te lang vestibulaire suppressiva hebben gebruikt, waardoor een goede compensatie en revalidatie wordt belemmerd.
Ze behandelt ook patiënten met bilateraal vestibulair verlies, hoewel minder vaak, ongeveer één geval per maand of om de paar maanden. Voor deze patiënten beginnen Claire en haar team met diagnostische tests en stellen vervolgens op maat gemaakte revalidatieprogramma's op. De oefeningen kunnen bestaan uit hoofdbewegingen en oogstabilisatietaken, strategieën voor visuele duizeligheid, balanstraining met schuimrubberen kussentjes, loop- of sta-oefeningen en oefeningen voor het hele lichaam. Patiënten worden aangemoedigd om deze oefeningen meerdere keren per dag gedurende korte periodes te doen, met regelmatige follow-ups om de voortgang te controleren en de moeilijkheidsgraad indien nodig te verhogen. Daarnaast worden, indien relevant, hulpmiddelen zoals een video over vestibulaire migraine aanbevolen.
Onder de belangrijkste uitdagingen De hoogtepunten van Claire zijn:
- Patiënten aanmoedigen om minder afhankelijk te worden van vestibulaire suppressiva.
- Het aanpakken van mobiliteits- of pijnproblemen, vooral bij oudere patiënten.
- Het beheren van lange wachtlijsten, met name voor vestibulaire fysiotherapie.
- Beperkte toegang tot geavanceerde apparatuur, zoals draaistoelen, die het verplaatsen van patiënten met mobiliteits- of rugproblemen tijdens tests zou vergemakkelijken.
Ondanks deze uitdagingen blijven Claire en haar team zich richten op het leveren van praktische, patiëntgerichte vestibulaire zorg.
Eerste ervaringen met de BalanceBelt
Claire hoorde voor het eerst over de BalanceBelt via Dr. Meehan, een audio-vestibulair arts die nu in een privépraktijk werkt. Dr. Meehan liet haar kennismaken met het apparaat en vroeg Claire om te helpen bij diagnostische tests en aanpassingen. Claire was geïntrigeerd en enthousiast om deze innovatieve technologie uit te proberen, omdat ze geloofde dat het echte voordelen zou kunnen bieden. Haar enige zorg in eerste instantie was of patiënten met een beperkte mobiliteit of bijkomende gezondheidsproblemen (zoals rugklachten) geschikte kandidaten zouden zijn.
Een van de eerste patiënten die ze behandelde was "Jenny", een plaatselijke vrouw met bilaterale vestibulaire stoornis na een luchtweginfectie. Jenny had sinds begin 2023 symptomen, met een lage score op alle zes de halfcirkelvormige kanaaltests en beperkte vooruitgang ondanks vestibulaire revalidatie. Toen ze naar Claire werd doorverwezen, was ze afhankelijk van een wandelstok of wandelstok en aanzienlijke fysieke ondersteuning van haar man, vooral buitenshuis.
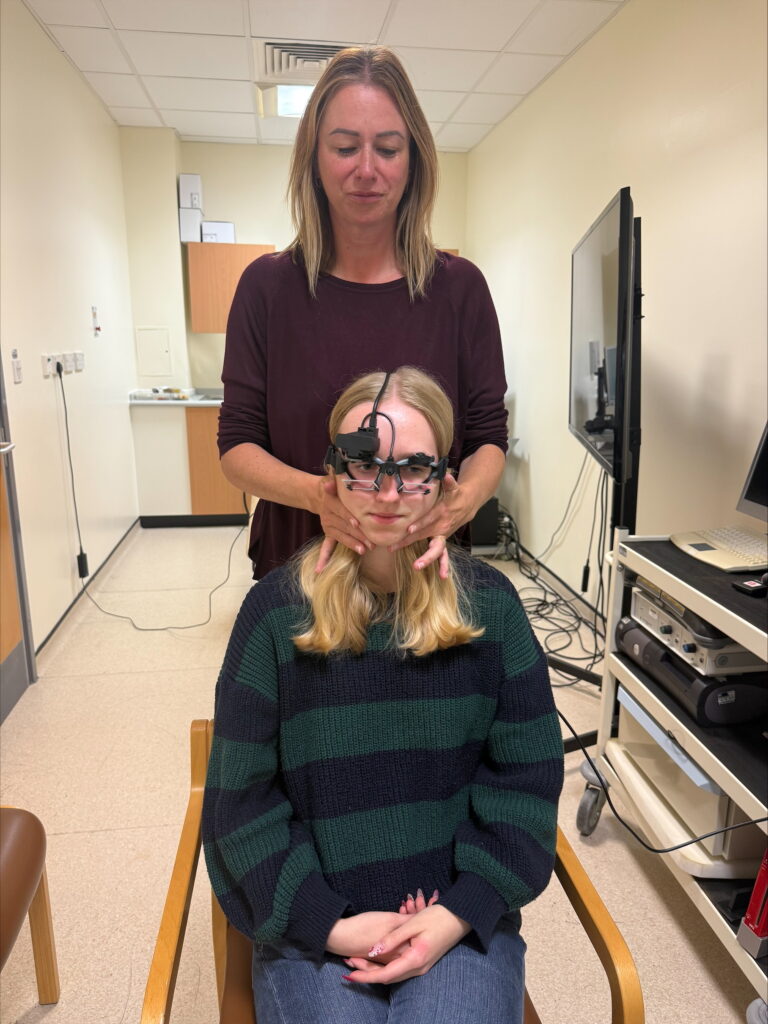
Tijdens de eerste beoordelingJenny voerde standaard sta- en looptests uit met en zonder de Balance Belt. Na slechts 15-20 minuten dragen gaf ze aan zich iets zelfverzekerder te voelen, hoewel de gemeten verbetering bescheiden was. Toch waren zelfs kleine vroege verbeteringen bemoedigend, gezien haar lange geschiedenis van symptomen.
Toen Jenny ongeveer drie weken later terugkwam, was het effect duidelijk: ze liep de kliniek binnen zonder zich aan de arm van haar man vast te houden en gebruikte haar wandelstok niet meer. Ze beschreef de riem als "van onschatbare waarde" Ze zei dat het haar angst om te vallen had verminderd, haar onafhankelijkheid had vergroot en haar in staat had gesteld om met meer zelfvertrouwen te lopen. Haar man merkte ook dat ze veel minder op hem leunde. Jenny kon zich zelfs weer vrijer in haar tuin bewegen, een betekenisvol teken van herwonnen onafhankelijkheid.
Bredere implicaties en conclusies
Vanuit haar eerste ervaringen ziet Claire een groot potentieel voor de BalanceBelt bij de behandeling van een breed scala aan vestibulaire patiënten, niet alleen die met bilateraal vestibulair verlies, maar ook unilaterale gevallen en iedereen die last heeft van afwijken of onvast lopen. Ze gelooft dat het een belangrijke rol kan spelen bij het verbeteren van mobiliteit, veiligheid en onafhankelijkheid bij verschillende patiëntengroepen.
Claire bracht ook de mogelijkheid ter sprake om het apparaat op te nemen in het Britse Toegang tot werk, een overheidsproject dat werknemers helpt bij het verkrijgen van praktische hulpmiddelen (zoals headsets of ringleidingsystemen) om effectief te kunnen blijven werken. De Balance Belt zou volgens haar op dezelfde manier kunnen worden aangeboden aan patiënten met evenwichtsstoornissen die hun vermogen om te werken belemmeren, wat zowel klinische als sociaaleconomische voordelen zou opleveren.
Wat betreft de volgende stappen benadrukte Claire de noodzaak van groter bewustzijn van de BalanceBelt onder clinici en patiënten. Ze staat open voor het behandelen van meer patiënten die zijn doorverwezen door BalanceBelt of door Dr. Meehan. Met het oog op de toekomst vroeg ze zich af hoe het apparaat zou kunnen worden geïntegreerd in de NHS, bijvoorbeeld door ziekenhuizen die riemen aanschaffen en deze voor een bepaalde behandelingsperiode aan patiënten uitlenen.