Het bericht The 5 Most Common Vestibular Disorders and What They Mean verscheen eerst op BalanceBelt.
]]>
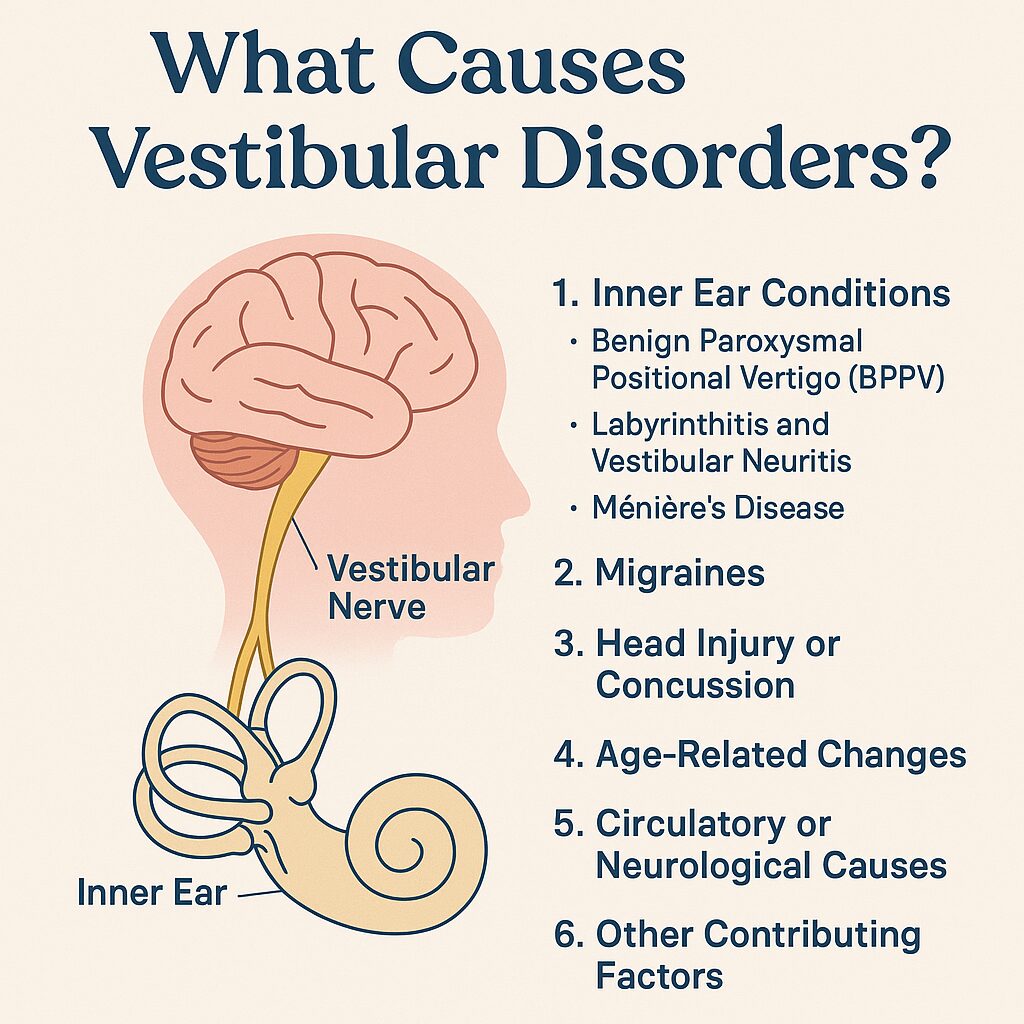
1. Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is one of the most common causes of vertigo. It occurs when tiny crystals in the inner ear move into the wrong place. You’ll usually feel a spinning sensation when you turn your head, roll over in bed, or look up. The good news? BPPV is treatable through specific head movements that guide the crystals back into place.
2. Meniere’s Disease
This condition causes episodes of vertigo, ringing in the ears, and temporary hearing loss. It is linked to fluid pressure changes in the inner ear. Managing salt intake, reducing caffeine, and controlling stress can help reduce the frequency and severity of attacks.
3. Vestibular Neuritis or Labyrinthitis
Caused by inflammation of the balance nerve—often after a viral infection—these conditions lead to sudden, intense dizziness that can last for days. Recovery may take time, and vestibular therapy can help the brain adapt and restore balance.
4. Vestibular Migraine
People with vestibular migraine experience dizziness and imbalance related to migraine activity, even without a headache. Sensitivity to light, motion sickness, and imbalance are common. Treatment focuses on migraine prevention, healthy routines, and managing triggers.
5. Bilateral Vestibular Hypofunction (BVH)
BVH occurs when both inner ears lose function, leading to constant imbalance and unsteady vision during movement. Walking in the dark or on uneven surfaces can be particularly challenging. Rehabilitation focuses on strengthening other senses to help compensate and improve stability.
Understanding Your Diagnosis
Knowing which type of vestibular disorder you have helps you make informed decisions about your care. Each condition has its own pattern, triggers, and treatment options, but all benefit from patience, movement, and support.
Living with a vestibular condition requires courage and adaptation, but it also opens the door to learning new ways to move through life with confidence and stability.
As this is the final blog from Stephanie for now, we want to thank her for sharing her knowledge and personal experience. If you’re looking for ways to feel steadier in your everyday activities, the Balance Belt may help you move more securely and confidently wherever you go.
Written by Stephanie Steggehuis | Marketing Copywriter living with BVH and Oscillopsia
Het bericht The 5 Most Common Vestibular Disorders and What They Mean verscheen eerst op BalanceBelt.
]]>Het bericht Into the Depths of Balance: The Story and Research of Physiotherapist Bart Zwaneveld verscheen eerst op BalanceBelt.
]]>What began with studying professional literature and attending conferences led by ENT specialists and neurologists gradually developed into a true specialization. Through contact with experts such as Herman Kingma, Raymond van de Berg, and Michael Strupp, his fascination with the vestibular domain grew. The gratitude of patients after receiving the correct treatment gave him the final push. This was the field in which he wanted to make a real difference.
From Student to Lecturer

Because many courses failed to answer his questions, Bart began teaching himself. Initially, he was asked “by accident” to give a short lecture; today, he is a highly sought-after lecturer throughout the Netherlands. His intrinsic motivation is to make high-quality, clinically relevant knowledge accessible to fellow physiotherapists.
Dizziness and balance disorders are fortunately receiving increasing attention, and Bart actively contributes through both master’s programs and national continuing education courses.
PhD Research on BPPD in Primary Care
Since the beginning of this year, Bart has been working on his PhD research, focusing on BPPD (Benign Paroxysmal Positional Dizziness). This condition causes dizziness when the head is moved suddenly, lasting from seconds to minutes, and is the most common cause of vertigo.
His research includes several components:
- Optimization of repositioning maneuvers by comparing parameters such as speed and execution
- Patient experience, including symptom intensity, nausea, and anxiety
- The role of explanation and counseling during testing and treatment
- Long-term outcomes and mapping residual symptoms
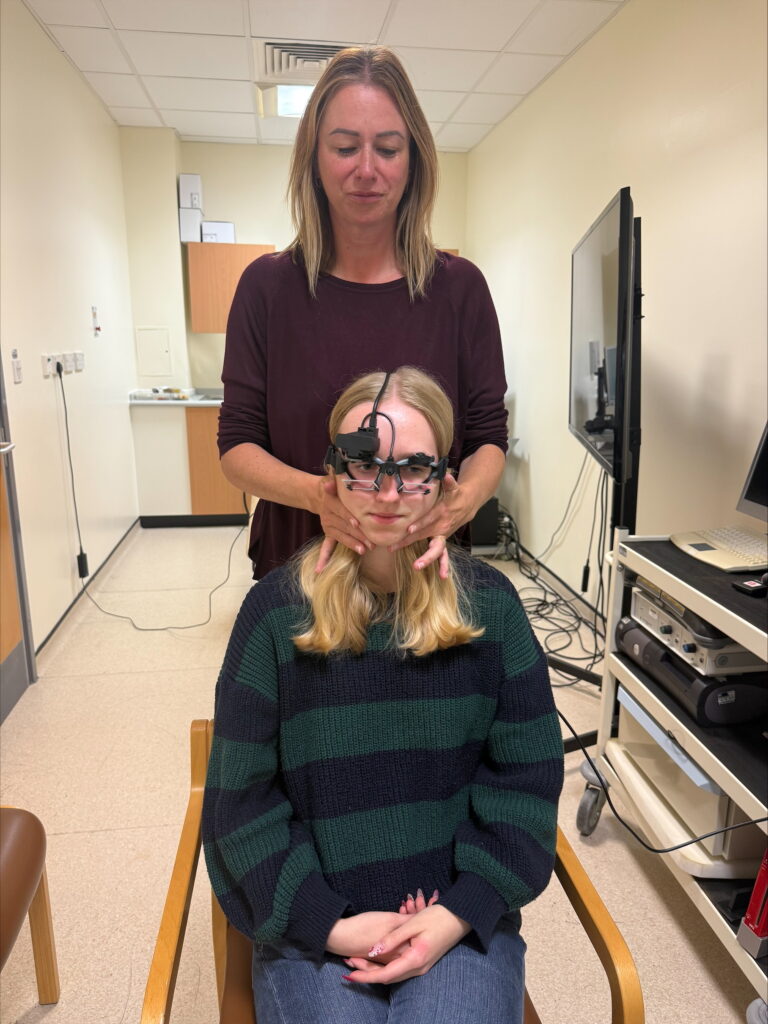
- Objective measurements using VNG (videonystagmography) to make vestibular testing as sensitive as possible in primary care
His mission is to make vestibular science accessible and practically applicable for primary care physiotherapists.
Daily Practice: Complex Vestibular Disorders
Through close collaboration with ENT specialists and neurologists, Bart treats a wide spectrum of patients. These include individuals with BPPD (often combined with other conditions), unilateral vestibular loss, Ménière’s disease, vestibular migraine, and bilateral vestibulopathy.
Many patients present only after months or even years of symptoms. Therefore, every treatment starts with careful diagnostics followed by extensive counseling. Understanding the condition gives patients an immediate sense of control.
The core of treatment often consists of vestibular rehabilitation: balance exercises, gaze stabilization and VOR (Vestibulo-Ocular Reflex) training, rebuilding confidence, and helping patients establish a “new normal.”
The BalanceBelt: A Valuable Addition

For some patients, rehabilitation alone is not sufficient. In these cases, the BalanceBelt can provide support. This belt uses subtle vibrations to provide information about body posture, helping the brain compensate more effectively.
Bart sees particular benefits for patients with:
- Bilateral vestibular loss
- Complex balance problems
- Patients for whom rehabilitation shows insufficient effect after three months
He primarily observes improvements in patients’ sense of safety, fatigue levels, mobility, independence, and overall quality of life.
An Impressive Case
One young patient with bilateral vestibular loss functioned like a very frail elderly person due to severe balance problems. Despite intensive rehabilitation, daily functioning remained extremely limited.
With the BalanceBelt, the patient’s fatigue decreased significantly, and he regained the confidence to go outside independently. Although it did not change his work disability status, it did restore his ability to function in daily life—an enormous improvement in quality of life.
Challenges and the Future
The greatest ongoing challenges remain making the correct diagnosis, providing emotional support, and helping patients truly understand their condition. Motivation among this patient group is high, which makes the work especially rewarding.
Bart enjoys thinking about future developments, whether it involves new applications such as vibrations at different frequencies or concepts like “balance socks” that provide feedback through the soles of the feet or calf muscles. Innovation in the field of balance never stands still.
A Mission for Better Care
Bart’s work in clinical practice, education, and research comes together in one clear ambition: improving care for patients with dizziness and balance disorders and making this care accessible throughout primary healthcare.
Through his research, teaching, and continuous pursuit of improvement, he contributes to this mission every day.
Het bericht Into the Depths of Balance: The Story and Research of Physiotherapist Bart Zwaneveld verscheen eerst op BalanceBelt.
]]>Het bericht Why healthy living matters even more when you have a vestibular condition verscheen eerst op BalanceBelt.
]]>Healthy living isn’t about being perfect. It’s about giving your body the best possible foundation to adapt and cope.
Your body’s foundation matters
Your brain and inner ear work closely together to keep you upright and oriented. For that communication to work well, your body needs a stable internal environment. Hydration, blood sugar levels, muscle strength, and overall energy all play a role in how your balance system performs.
When your body is well nourished and well rested, your brain can focus on adapting to changed balance signals instead of constantly trying to compensate for fatigue, stress, or low energy. Small things — like drinking enough water or eating regularly — can have a surprisingly big impact on how you feel.

Movement helps the brain adapt
When you live with a vestibular condition, movement can feel uncomfortable or even scary. But gentle, consistent movement is one of the most powerful tools you have. Every time you move, your brain gets another opportunity to learn how to deal with altered balance input.
This doesn’t mean pushing through severe symptoms. Start small and safe. A short daily walk, light stretching, or simple balance exercises can already support adaptation. Over time, these small movements help rebuild confidence and improve stability. Always listen to your body and move at your own pace
Food and rest are key
What and when you eat matters. Try to eat regular meals, include enough protein, vegetables, and healthy fats, and avoid long gaps between meals. Poor nutrition or dehydration can intensify dizziness, fatigue, and unsteadiness.
And don’t underestimate sleep. Your brain does a lot of its processing, recovery, and adaptation while you rest. Good sleep won’t cure a vestibular condition, but it can make your symptoms more manageable and your days more predictable.
Taking care of your mind
Living with dizziness, imbalance, or visual disturbances can be mentally exhausting. Stress and anxiety often amplify vestibular symptoms, creating a difficult cycle.
Finding small moments of calm can help break that cycle. This might be meditation, breathing exercises, journaling, reading, or talking to someone who truly understands what you’re going through. The goal isn’t to eliminate stress completely, it’s to manage it in a way that supports your recovery.

A healthy routine gives you back control
A vestibular condition can make you feel like your body is no longer predictable. Healthy routines help restore a sense of control. While you can’t always control your symptoms, you can control how you support your body every day.
Over time, those small, consistent choices add up. They can help you feel stronger, steadier, and more confident in daily life.
If you’re looking for extra support while rebuilding those habits, tools like the BalanceBelt can help you move more safely and confidently, step by step, as your brain continues to adapt.
Written by Stephanie Steggehuis Marketing Copywriter living with BVH and Oscillopsia
Het bericht Why healthy living matters even more when you have a vestibular condition verscheen eerst op BalanceBelt.
]]>Het bericht Why fatigue with a vestibular disorder feels so overwhelming. verscheen eerst op BalanceBelt.
]]>What’s really happening

Your vestibular system normally tells your brain where you are in space. When it’s not working properly, your brain has to rely on your eyes and your body’s sense of position to fill in the blanks. That constant effort takes energy. Every movement, every head turn, every change in lighting or noise is extra work for your brain to process.
Fatigue is more than physical
It’s not just your body that feels drained. Your mind can too. Simple tasks like grocery shopping or scrolling on your phone can leave you foggy or irritable. The emotional side of fatigue can be just as tough as the physical side. You might feel frustrated, isolated, or even guilty for not being able to do as much as you used to.
What helps?
Some things that may help:
- Try to see fatigue as your body’s way of asking for balance, not weakness.
- Keep a journal to track when your energy dips, and look for patterns.
- Pace your day by mixing active moments with quiet breaks.
- Prioritise sleep and create small routines that help you wind down.
- Eat nourishing foods and stay hydrated to support your body’s recovery.
- Move regularly, as long as it feels safe and is guided by a professional who understands vestibular conditions.
- And most importantly, remind yourself that rest is not a luxury. It’s part of recovery.

You’re not lazy, you’re adapting
Fatigue doesn’t mean you’re doing something wrong. It means your brain and body are working harder than most people’s just to keep you standing and focused. Give yourself permission to rest without guilt.
If you’re looking for ways to feel more balanced and less exhausted as you go about your day, the Balance Belt could help ease some of that extra effort so you can focus on living again.
Written by Stephanie Steggehuis | Marketing Copywriter living with BVH and Oscillopsia
Het bericht Why fatigue with a vestibular disorder feels so overwhelming. verscheen eerst op BalanceBelt.
]]>Het bericht From Constant Coping to Actually Living Again – Thanks to the BalanceBelt. verscheen eerst op BalanceBelt.
]]>
In 2001, Mrs. De Vries first began experiencing balance problems. It started with mild but persistent dizziness. “I never fell, and I never felt truly nauseous, but it did limit me in my daily life,” she explains. “At work, I had several long periods of sick leave, which was difficult. I really loved my job.”
At the time, she worked in psychosocial support and education at a regional cancer center. “I organized meetings for doctors, nurses, and other healthcare professionals to improve education and psychosocial care for cancer patients. It was work that meant a lot to me.”
However, as her symptoms progressed, her work became increasingly difficult to maintain. “I saw several ENT doctors—first in Den Bosch and later in Eindhoven—and they diagnosed Ménière’s disease. Eventually, I ended up with Professor Kingma in Maastricht. He determined that I had bilateral vestibular hypofunction. The explanation of what that meant hit hard, but it also gave clarity.”
In 2009, she had to stop working completely. “That was very difficult, because my work was a big part of my identity. But I simply couldn’t continue. What followed was a long period of searching, accepting, and learning to live with my limitations.”
A Long Road to Acceptance
The years that followed were dedicated to adapting to a new reality. “I was never afraid to go outside. I went for walks using a cane, because I wanted to keep enjoying nature.”
After a difficult period of grief and fatigue, she slowly found more stability around 2015. “With psychological support and physiotherapy-guided exercise, I gradually regained some balance. I learned to plan my days very carefully: resting the day before an activity and spending two days recovering after. Everything had to be done with caution. That worked—but it limited my life enormously.”
A Chance Discovery
It wasn’t until late August 2025 that she came across the BalanceBelt—completely by coincidence.
“I was searching online for a video to explain my balance disorder to my French son-in-law. That’s how I found the BalanceBelt. I thought: I want to try that! Even though I had just become a widow and was in a difficult emotional period.”
The First Weeks With the Belt
She contacted the BalanceBelt team and was referred to a physiotherapist in Nijmegen. “I travelled to my first appointment without a cane, by train and then by bus — to the physiotherapist’s surprise. I am seemingly just mobile, so people do not see that I have balance problems.”
During that first appointment, she didn’t notice much difference yet. The real change came once she started using the belt in her daily life.
A few days later, she went on a weekend trip with her daughter and son-in-law. “We walked three days in a row, went out for dinner, visited a city, and did some shopping. Normally, I would have been exhausted afterwards. But when I got home, I thought: Where is the fatigue? My daughter even said: ‘I think we are more tired than you are!’”
She could hardly believe it. “A week later, I walked with a friend in the dark, without a cane, on uneven ground. I waited for the fatigue to set in—but it didn’t. That’s when I knew: this really works.”
More Energy, More Freedom
Since using the BalanceBelt, her life has changed dramatically. “I have more energy, more days in the week. I used to have only two or three functioning days — now I have all seven. My mind feels calmer, I sleep better, I enjoy the world around me again.”
Even cycling short distances has become easier. “Before, I had to focus all my attention on cycling. Now I can look around and enjoy the ride.”
The effect is subtle, but powerful. “The belt has made my life so much richer. I can spend my energy on living instead of just coping. I have room in my head again.”
Enjoying Life Again

Over the years, she had adapted her hobbies. From long walks and attending concerts, she moved to more seated activities such as sewing and drawing. “I design Arabic patterns; I make birth cards and birthday cards. If I ran out of energy, I could just stop and continue the next day.”
Now, with more energy, she can slowly rediscover what she wants her days to look like. “That will take some time — I’ve lived more than 20 years with limitations.”
She smiles: “I’m 75, but I feel more active than I have in years. Instead of slowing down, I’m becoming more energetic again. People say I’m glowing. And they’re right — I have all seven days of the week back!”
Het bericht From Constant Coping to Actually Living Again – Thanks to the BalanceBelt. verscheen eerst op BalanceBelt.
]]>Het bericht The hardest part of Bilateral Vestibular Hypofunction isn’t the symptoms…. it’s feeling like you’ve lost yourself verscheen eerst op BalanceBelt.
]]>
When you first get a diagnosis like Bilateral Vestibular Hypofunction (BVH) or any vestibular condition, you expect dizziness, balance issues, maybe nausea. What you don’t expect is how deeply it changes how you feel about yourself. The hardest part often isn’t the physical symptoms. It’s realising that you’re not the same person you used to be.
The loss no one talks about
You might remember walking easily through a store, chatting with friends in a busy café, or driving without thinking twice. Now, things that used to feel effortless can seem impossible. It’s not just frustrating, it’s heartbreaking. BVH happens when both sides of your inner ear stop sending the right signals to your brain. That means your brain has to work much harder to keep you balanced, and every movement takes extra effort.
More than physical
The emotional side of vestibular disorders doesn’t get talked about enough. You’re grieving the version of yourself who could do things freely and confidently. Many people with BVH say that feeling “different” or “not themselves anymore” is harder to accept than the dizziness itself. It’s a strange kind of loss, because on the outside you look the same, but inside everything feels different.
Learning to live as the new you
Healing starts when you stop comparing yourself to who you were. That doesn’t mean you’re giving up. It means you’re allowing yourself to grow into a new version of you. A version that still deserves joy, confidence, and independence.
Try small steps that rebuild trust in your body. Work with a vestibular therapist to help your brain adjust. Make your home safer and easier to move around in. Be honest with friends and family about what you’re feeling. And most of all, be kind to yourself. Progress can be slow, but it’s still progress.
Finding yourself again

You might never go back to exactly who you were, but that doesn’t mean you can’t feel like yourself again. You’re still you, just with a different balance system. And with time, patience, and the right support, you can start to feel steady and confident again.
If you’d like to explore tools that can help you feel more stable and more like yourself, the BalanceBelt may help you regain confidence in your daily life.
The journey to adjustment can be challenging, but you’re not alone. In the next post, Stephanie will explore why fatigue with a vestibular disorder feels so overwhelming, helping you understand one of the most common yet often invisible challenges.
Written by Stephanie Steggehuis | Marketing Copywriter living with BVH and Oscillopsia
Het bericht The hardest part of Bilateral Vestibular Hypofunction isn’t the symptoms…. it’s feeling like you’ve lost yourself verscheen eerst op BalanceBelt.
]]>Het bericht “The BalanceBelt finally offers patients with severe balance loss something to be hopeful about.” – Prof. Dr. Raymond van de Berg verscheen eerst op BalanceBelt.
]]>
At Maastricht UMC+, ENT specialist Dr. Raymond van de Berg has been working for years with patients suffering from severe balance disorders. “In the Netherlands, we’re basically the ‘last resort’ for people with complex balance problems,” he explains. “Patients come to us from all over the country, and even from abroad, because the expertise is concentrated here.”
Alongside his clinical work, Van de Berg is deeply involved in research on vestibular disorders, from diagnostics to innovative treatments such as the artificial balance organ and the BalanceBelt.
The power of interdisciplinary thinking
What drives him in this field? “Balance disorders are incredibly fascinating because they sit at the crossroads of ENT, neurology, ophthalmology, psychiatry, and even physics,” says Van de Berg enthusiastically. “It’s an area where logical reasoning, technology, and clinical experience all come together.”
The BalanceBelt: from idea to impact
Van de Berg became involved with the BalanceBelt through Prof. Herman Kingma, a pioneer in balance research and the inventor of the technology behind the belt.
“In the beginning it was still a university project, but since the collaboration with Elitac Wearables, it has become truly professional,” he says.
The initial experiences with the BalanceBelt were very promising. “Some patients were absolutely ecstatic; others noticed less difference. But what stood out most is that there’s a group of patients who continue using the belt consistently, even after two years. That says something about the value they experience.”
According to Van de Berg, the BalanceBelt works particularly well for patients with severe bilateral vestibular loss, people who have literally lost their sense of balance. “In addition, there seems to be a subgroup of patients with an oversensitive balance system, such as those with 3PD (Persistent Postural-Perceptual Dizziness). For them, the belt mainly helps to restore confidence in their own balance system.”
Challenges and improvements
While he is enthusiastic, Van de Berg also sees challenges ahead. “The biggest one remains distinguishing the true medical effect from the placebo effect. That’s important for recognition, reimbursement, and further scientific validation.”
He also sees room for technical improvement: “The price is still a barrier. And beyond that, we could think of faster feedback, lighter materials, and more individualized settings for each patient.”
The Vestibular Implant (VI): taking the next step
In addition to research on the BalanceBelt, Maastricht UMC+ is also developing the Vestibular Implant (VI), an artificial balance organ. “It’s an implant that, just like a cochlear implant for hearing — electrically stimulates the vestibular nerve,” Van de Berg explains. “In that way, we aim to partially restore the reflexes of the balance organ.”
The potential is huge, but the road is long. “Ten years ago, we thought: within five to ten years this will be ready for patients. And now we’re still saying the same, mainly because of European regulations. The technology is there, the doctors are ready, the patients are ready, but the administrative barriers are enormous.”
Two technologies, each with its own role
How does Van de Berg see the relationship between the BalanceBelt and the Vestibular Implant? “The main difference is that the VI primarily restores reflexes, while the BalanceBelt supports balance. For many patients, that distinction is crucial: those who mainly suffer from balance instability can already benefit greatly from the BalanceBelt. The VI is a surgical option, something for later, or for patients with very severe loss.”
He even sees potential synergy between the two technologies in the future. “Who knows, they might complement each other. The BalanceBelt could be the first step, and the implant the second.”
Raising awareness is key
According to Van de Berg, there’s still much to be gained by improving awareness and diagnosis of balance disorders. “There are still many people walking around with bilateral vestibular loss without realizing it. Doctors and patients often don’t consider the balance system as the root cause. Greater awareness among general practitioners, ENT specialists, neurologists, and patients themselves is crucial.”
“Every step forward counts”
Van de Berg concludes on an optimistic note: “Whether it’s with an implant or with the BalanceBelt, every step that helps people with balance disorders move with confidence again is a victory. And that’s what we work on every day here in Maastricht.”
Het bericht “The BalanceBelt finally offers patients with severe balance loss something to be hopeful about.” – Prof. Dr. Raymond van de Berg verscheen eerst op BalanceBelt.
]]>Het bericht Reclaiming independence: Interview with Claire Snape on BalanceBelt impact. verscheen eerst op BalanceBelt.
]]>
By chance, a colleague suggested audiology, and at that time, in 1997, the profession could still be entered through an apprenticeship rather than a university degree. Claire seized the opportunity, training at the School of Audiology in Nottingham and combining hands-on clinical work with medical physics studies at People’s College. The apprenticeship route not only gave her direct clinical exposure from day one but also spared her university tuition fees.
She went on to build her career in Nottingham before moving to Derby in 2004, where her focus expanded beyond hearing aids into vestibular diagnostics and rehabilitation. Today, Claire works as part of a dedicated multidisciplinary team, delivering comprehensive balance and hearing care, and helping to develop streamlined clinics that bring together audiologists and ENT specialists for patient-centered solutions.
The Patients and Challenges of Vestibular Care
Claire explains that the types of patients she sees have changed over time. In the past, cases of labyrinthitis and vestibular neuronitis were more common, but recently she has noticed a rise in patients with Persistent Postural-Perceptual Dizziness (PPPD). These patients are often more complex, as they may have been on vestibular suppressants for too long, preventing proper compensation and rehabilitation.
She also sees patients with bilateral vestibular loss, though less frequently, around one case per month or every couple of months. For these patients, Claire and her team begin with diagnostic testing and then design tailored rehabilitation programs. Exercises may include head movement and gaze-stabilization tasks, visual-vertigo strategies, foam pad balance training, walking or standing routines, and whole-body exercises. Patients are encouraged to practice these exercises for short periods multiple times a day, with regular follow-ups to monitor progress and increase difficulty as needed. Additionally, resources such as a vestibular migraine video are recommended when relevant.
Among the main challenges Claire highlights are:
- Encouraging patients to reduce reliance on vestibular suppressants.
- Addressing mobility or pain issues, especially in elderly patients.
- Managing long waiting lists, particularly for vestibular physiotherapy.
- Limited access to advanced equipment, such as rotating chairs, which would make repositioning tests easier for patients with mobility or back problems.
Despite these challenges, Claire and her team remain focused on delivering practical, patient-centered vestibular care.
First Experiences with the BalanceBelt
Claire first learned about the BalanceBelt through Dr. Meehan, an audio-vestibular physician who now works privately. Dr. Meehan introduced her to the device and asked Claire to support with diagnostic testing and fittings. Claire was intrigued and excited to try this innovative technology, believing it could offer real benefits. Her only initial concern was whether patients with poor mobility or additional health issues (like spinal problems) would be suitable candidates.
One of the first patients she fitted was “Jenny”, a local woman with bilateral vestibular failure following a respiratory infection. Jenny had been symptomatic since early 2023, with low gain on all six semicircular canal tests and limited progress despite vestibular rehabilitation. By the time she was referred to Claire, she relied on a cane or walking pole, and significant physical support from her husband, especially outdoors.
During the initial assessment, Jenny performed standard standing and walking tests with and without the Balance Belt. After just 15–20 minutes of wearing it, she reported feeling slightly more confident, though the measured improvement was modest. Still, given her long history of symptoms, even small early gains were encouraging.
When Jenny returned about three weeks later, the impact was clear: she walked into the clinic without holding her husband’s arm and was no longer using her walking stick. She described the belt as “invaluable,” saying it had reduced her fear of falling, increased her independence, and allowed her to walk more confidently. Her husband also noticed she relied on him much less. Jenny even regained the ability to move more freely around her garden, a meaningful sign of restored independence.
Broader Implications and Takeaways
From her first experiences, Claire sees strong potential for the BalanceBelt in treating a wide range of vestibular patients, not only those with bilateral vestibular loss, but also unilateral cases and anyone experiencing veering or unsteady walking. She believes it could play an important role in improving mobility, safety, and independence across different patient groups.
Claire also raised the possibility of incorporating the device into the UK’s Access to Work, a governmental project, which helps employees secure practical aids (such as headsets or loop systems) to continue working effectively. The Balance Belt, she suggested, could similarly be offered to patients whose vestibular disorders interfere with their ability to work, providing both clinical and socioeconomic benefits.
As for next steps, Claire highlighted the need for greater awareness of the BalanceBelt among clinicians and patients. She is open to fitting more patients referred either by BalanceBelt or by Dr. Meehan. Looking ahead, she wondered how the device could be integrated into the NHS, perhaps with hospitals purchasing belts and loaning them to patients for defined treatment periods.
Het bericht Reclaiming independence: Interview with Claire Snape on BalanceBelt impact. verscheen eerst op BalanceBelt.
]]>Het bericht BalanceBelt featured in Meniere’s Society and Spin Magazine verscheen eerst op BalanceBelt.
]]>We’re excited to share that the BalanceBelt has recently been featured by the Meniere’s Society.
Earlier this year, our article was published on their website: Read it here.
In this article you can read for whom the BalanceBelt is suitable, which problems they experience, what the BalanceBelt does, and how it is available in the UK.

Now, the story has also appeared in their magazine, Spin. You can find the online version here: Spin Magazine.
The magazine also describes how Professor Herman Kingma, after seeing a patient with severe BVL in 2003, developed the BalanceBelt to address the lack of treatment options. Clinical studies show that many BVL patients benefit, experiencing improved mobility, reduced anxiety, and a higher quality of life. Impressively, 80% noticed positive effects after just two hours of use, and some even returned to cycling.
Het bericht BalanceBelt featured in Meniere’s Society and Spin Magazine verscheen eerst op BalanceBelt.
]]>Het bericht Meet Claire Potter: Specialist in Vestibular Physiotherapy verscheen eerst op BalanceBelt.
]]>
Claire Potter is a dedicated vestibular physiotherapist at a central London trust. Her journey into physiotherapy was inspired by a personal experience, her mother’s recovery from a serious knee injury through physiotherapy. Initially interested in musculoskeletal care, Claire soon found her passion in neurological rehabilitation, eventually specialising in vestibular physiotherapy over the past three and a half years.
Working with patients suffering from chronic balance disorders, some with symptoms lasting up to 20 years, Claire finds reward in both the complexity and the life-changing potential of her field. From treating Benign Paroxysmal Positional Vertigo (BPPV), often with immediate results, to supporting those with Persistent Postural-Perceptual Dizziness (PPPD) and Functional Neurological Disorder (FND), her work blends science, empathy, and collaboration with psychology. Her enthusiasm for meaningful, measurable outcomes makes her a strong advocate for tools like the BalanceBelt.
Pushing Boundaries Despite Limited Resources
Claire is deeply committed to improving patient outcomes, yet she acknowledges the constraints of working within the NHS. While complex vestibular cases, particularly patients with conditions like PPPD or Functional Neurological Disorder, can benefit greatly from long-term care, NHS resources often limit treatment provision within the confines of economic viability. In her private practice, she has seen how patients thrive with extended care, highlighting a gap in what public services can currently provide.
Despite these limitations, Claire is grateful to be part of a well-resourced and forward-thinking team. The multidisciplinary team (MDT) includes consultants, audiologists, and a strong cohort of physiotherapists, all supported by an encouraging management team. This collaborative environment enables continued professional development, networking, and active involvement in clinical research.
The service has evolved significantly in the past decade, particularly during COVID, to embrace remote care and increase patient access. Claire and her colleagues are also working to elevate their service to a national center of excellence.
Treating Severe Vestibular Disorders: A Holistic, Structured Approach
Claire explains that treating patients with severe vestibular dysfunction, particularly those with bilateral vestibular loss, is highly complex and must be tailored to different subgroups. Some patients come with rare conditions like Neurofibromatosis type 2 (NF2), while others suffer from age-related decline or unexplained progressive vestibular loss in midlife. These individuals often experience debilitating symptoms such as oscillopsia, veering while walking, and repeated falls, often after years of misdiagnoses and specialist referrals.
For this group, Claire emphasises a holistic and psychologically sensitive approach. Many patients arrive feeling demoralised, especially once they understand their condition is chronic. Initial treatment includes reviewing vestibular test results, discussing home and environmental modifications (e.g., better lighting, removing rugs), and introducing strategies to manage anxiety and fear of falling.
Rehabilitation plans typically include daily walking routines and balance training exercises to optimise the 3 balance systems.
Until recently, Claire notes, options beyond this core rehab program were scarce, a gap that new tools like the BalanceBelt could help fill.
Introducing the BalanceBelt: From Cautious Curiosity to Clinical Impact

Claire Potter first learned about the BalanceBelt through her clinic’s monthly journal club, where her team discussed one of the early research papers. At the time, they viewed the device with interest but caution, assuming it would be difficult to introduce into the NHS without more robust data. However, a hands-on demonstration at a professional event (ACPIVR) changed that. After trying the belt herself and receiving a trial unit from the BalanceBelt team, she took the initiative to lead internal testing.
Initially skeptical, Claire questioned whether the device’s non-directional vibratory feedback would be tolerated or helpful for patients. However, given the lack of alternative treatment options for complex bilateral vestibular loss, she decided it was worth trying. The clinical rationale was: “It can’t hurt, and if it helps, that’s a win.” She began trialing the belt on selected patients under strict agreements, making it clear they would need to self-fund if they found it beneficial.
Interestingly, one patient with a functional neurological disorder (FND) felt worse when the belt was active, but better simply wearing it, suggesting that even the physical presence of the device may enhance truncal awareness for some. This highlighted the nuanced ways the belt might interact with different pathologies, especially in patients prone to sensory hyper-awareness or internalisation.
Despite that outlier, Claire reports that most patients with bilateral vestibular hypofunction showed clear improvement. One woman, who had not been able to run for three years, was so moved by her restored ability that she cried during the session. Such moments reinforced the belt’s potential to offer life-changing outcomes when used appropriately.
Case Summary: The Impact of the Balance Belt on a Patient with Severe Vestibular Dysfunction
A patient in her 50s was referred to the balance clinic by her GP, following a history of debilitating vestibular symptoms, including oscillopsia and profound imbalance. She had become unable to drive, leaving her socially isolated and dependent on her husband for mobility. The impact on her personal life was significant, she could no longer care for her two teenage children as she once had, and she experienced panic attacks and anxiety due to her condition.
Upon referral, she was assessed in the multidisciplinary team (MDT) balance clinic, which includes physiotherapists, audiologists, and medical specialists. Diagnostic testing revealed bilateral vestibular hypofunction affecting both semicircular canals and otolith organs. Initial physiotherapy focused on home safety, gentle balance exercises, and lifestyle adaptations, including a referral for occupational health support. However, progress was limited, and her symptoms remained highly provoking.

A pivotal moment came with the introduction of a BalanceBelt despite sizing limitations, the belt provided immediate and visible improvement. During outcome testing, which included mobility and confidence assessments, her performance improved significantly. Notably, she no longer clung to her husband’s arm and was visibly more confident, even smiling for the first time in therapy.
Although the belt did not address all symptoms (e.g. oscillopsia), it successfully boosted her confidence and allowed her to begin re-engaging in physical activity and daily routines. The team emphasised setting realistic expectations for the device: while it does not restore vestibular function, it serves as a powerful adjunct to help patients regain independence and improve quality of life.
Summary: Clinical Insights and Future Implications of the Balance Belt
The BalanceBelt does not replace or restore the vestibular system itself, it does not resolve symptoms like oscillopsia or directly substitute vestibular input. However, what it does, is provide an adjunctive sensory cue that improves confidence, postural control, and functional mobility, making it particularly valuable for patients with bilateral vestibular hypofunction.
Claire notes that the belt could also benefit individuals with unilateral vestibulopathy, especially when one side is severely affected, and compensation is limited. Furthermore, it may have potential applications for patients with persistent postural-perceptual dizziness (PPPD) and other chronic balance disorders but further research is required.
Importantly, Claire emphasises the need for careful patient selection and setting realistic expectations. Future implementation should be backed by further clinical trials and research to identify which subgroups will benefit most. Despite the need for more evidence, the early results suggest the BalanceBelt could fill a critical gap in treatment where current medical and physiotherapy options are limited.
Het bericht Meet Claire Potter: Specialist in Vestibular Physiotherapy verscheen eerst op BalanceBelt.
]]>